The F.M. Kirby Neurobiology Center is fully committed to recruiting and supporting talented individuals and ensuring they all have a place in our research community.
Neuroscience Research at Kirby
We are proud to be working at the vanguard of basic and translational neuroscience research within a world-class hospital research setting at Boston Children’s Hospital. We take full advantage of the exceptional breadth of Harvard’s neuroscience enterprise. Multidisciplinary collaborations and access to world class facilities ensure best in class application of genetics, genomics, molecular, cell, systems and behavioral neurobiology, and stem cell science, all colored by clinical insights. We aim to expand knowledge about the development and function of the brain, to understand what goes wrong in neurological and psychiatric diseases, and to contribute to their therapies and cures.
Here are a few cases that illustrate the broad scope of the basic and translational work by faculty in the Kirby Center.
Alban Latremoliere, Boston Children’s Hospital, Johns Hopkins
Featured Publications:
Nature (September 2018)
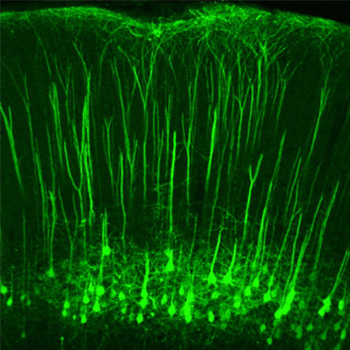
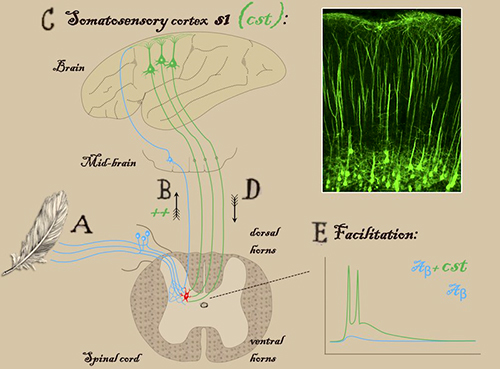
Touch and tactile neuropathic pain sensitivity are set by corticospinal projections
Vector (September 2018)
Neurons from the brain amplify touch sensation. Could they be targeted to treat neuropathic pain?
Vector (February 2018)
Deconstructing neuropathic pain: Could it give clues to better drugs?
Vector (October 2017)
Can rare pain syndromes point the way to new analgesics?
Vector (September 2018)
Overcoming pain by tackling the fear factor
Parsing Pain
Pain is a survival mechanism when it alerts us to danger in our environment. But, too often, pain can take on a life of its own, threatening our health and wellbeing, and constitute a disease in itself.
FM Kirby Center Director and Harvard Medical School professor of neurobiology and neurology at Boston Children’s Hospital, Dr Clifford Woolf, has devoted a career to understanding the basic neurobiological mechanisms of pain and to help spark the development of more effective therapies to alleviate pain, especially ones that don’t have the abuse potential of opioids. Woolf works on pain and on the regeneration and degeneration of the nervous system, with a particular focus on neurological disease modeling and drug screening in patient iPS-cell-derived neurons.
At Boston Children’s Hospital, Woolf has pioneered the use of human stem cell neurons to study pain, ALS and regeneration. Woolf and his collaborators at the Harvard Stem Cell Institute have developed human pain sensing neurons, a major advance in the study of pain, disease modeling, and development of innovative treatments. He has also contributed to the appreciation that sensory neurons contribute to certain inflammatory conditions via neuroimmune interactions. His work has been devoted to taking a more mechanistic approach to the study of pain and into translating this into new therapies, especially by inhibiting key pain promoting modulators and by selectively silencing pain signaling.
Dr Woolf’s research has inspired collaborations across academic centers and hospitals, as well as commercial biotech and pharmaceutical laboratories.
Zhang et al., 2018, Neuron 99, 1–13, July 25, 2018
Michael Crickmore, PhD, Bibliography
Featured Publications:
Neuron (July 2018)
Motivation, Perception, and Chance Converge to Make a Binary Decision.
Vector (June 2015)
Fruit flies’ love lives could clarify brain cells’ role in motivation
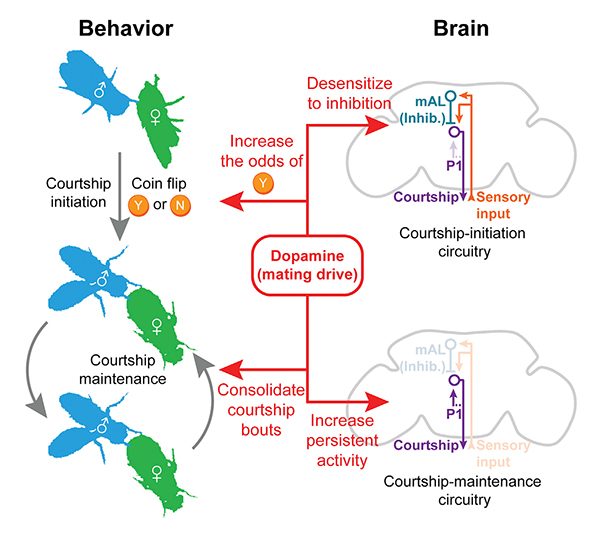
Hacking Motivation
Motivational states — drives for food, reproduction, temperature control, sleep, etc. — are the brain’s way of matching our behaviors to our needs. We eat when we’re hungry and sleep when we’re sleepy, but forego both when other things seem more important. Motivational states are fundamental tools bestowed by evolution to ensure our survival. In our modern world, motivations can often spiral out of control, and instead of bringing balance to our lives, lead to addictions or other disorders of behavior and mood.
Michael Crickmore, PhD, a principal investigator at the Kirby Center and Assistant Professor of Neurology at Boston Children’s Hospital, is undertaking a widespread investigation of the basic neurobiology behind drives decision making. The Crickmore Lab uses the small brain of the fruit fly, Drosophila melanogaster, focusing on the ~3,000 neurons that control the many motivations and decisions that differ between males and females. They have identified several circuit elements (small groups of neurons) that perform motivational functions, including neurons that send and receive dopaminergic signals, which also control human motivations. This is just one of the many indications that their molecular and circuit level discoveries will help us understand our own motivations in sickness and in health.
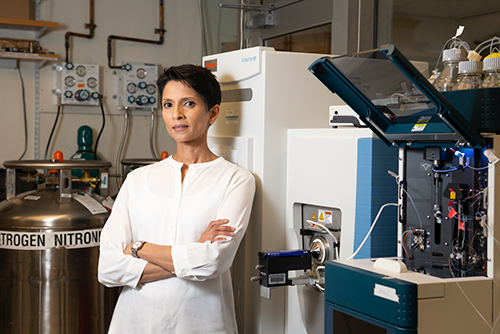
Photo by Anna Olivella, courtesy of the Harvard Brain Science Initiative.
Judith Steen, PhD, Bibliography.
Featured Publications:
Analytical Chemistry (April 2016)
FLEXITau: Quantifying Post-translational Modifications of Tau Protein in Vitro and in Human Disease
Molecular & Cellular Proteomics (October 2015)
MStern Blotting-High Throughput Polyvinylidene Fluoride (PVDF) Membrane-Based Proteomic Sample Preparation for 96-Well Plates.
Nature Methods (April 2012)
FLEXIQinase, a mass spectrometry-based assay, to unveil multikinase mechanisms.
Detecting Alzheimer’s
AD is the sixth leading cause of death in the United States. To date, diagnosis of the disease remains relatively subjective, based on observations of mental decline. By the time a patient’s function is noticeably impaired, irreversible brain changes and damage have already occurred.
Dr Steen and her colleagues deploy mass spectrometry, proteomics, and bioinformatics to analyze and characterize factors related to neurological diseases. neurodegeneration, and injury. The Steen laboratory uses a large-data approach, applying large “Omics” datasets of human brain tissues and body fluids from pathologically well-characterized patient cohorts. These terabytes of data are then mined with machine learning and other computational methods to help us to identify key molecular features of disease. The purpose of the work is to find biomarkers and therapeutic targets for neurodegenerative disease. Key to Steen’s work is the study of human tissues and fluids, thus avoiding any translational gap.
One of the promising directions emerging from this work is the identification of biomarkers to aid in the early diagnoses and treatment for Alzheimer’s Disease (AD) and other dementias including Frontotemporal Degeneration and Dementia with Lewy Bodies. Biomarkers, short for biological markers, are biological signals detected by blood and urine tests. With more enigmatic and devastating diseases, like Alzheimer’s, the related biomarkers have long eluded researchers. When relatively non-invasive and inexpensive biomarkers become available, a simple test in a doctor’s office could reveal a patient’s probability for developing AD early enough to apply preventive measures. Biomarkers could ultimately determine which therapies would be most effective for individual patients.

Members of the Stevens Lab in microglia formation, Boston Children’s Hospital
Beth Stevens, PhD, Bibliography
Featured Publications:
Immunity (April 2019)
“Immune Signaling in Neurodegeneration”
Immunity (January 2019)
“Single-Cell RNA Sequencing of Microglia throughout the Mouse Lifespan and in the Injured Brain Reveals Complex Cell-State Changes”
Nature “News and Views” (February 2018)
“Pruning Hypothesis Comes of Age”
Science (May 2016)
“Complement and microglia mediate early synapse loss in Alzheimer mouse models”
The New Yorker, (March 2016)
“Runs in the Family: New findings about schizophrenia rekindle old questions about genes and identity”
The New York Times (January 2016)
“Scientists Move Closer to Understanding Schizophrenia’s Cause”
Neuron (May 2012)
“Microglia Sculpt Postnatal Neural Circuits in an Activity and Complement-Dependent Manner”
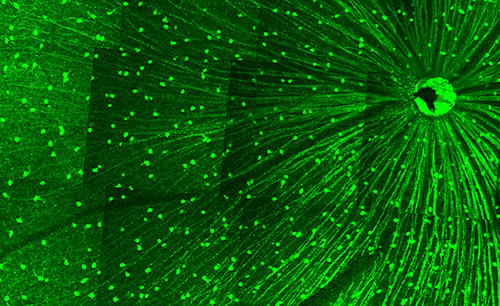
Pruning Synapses
Beth Stevens, PhD, is Research Associate in Neurology, Boston Children’s Hospital; Investigator, Howard Hughes Medical Institute; Associate Professor of Neurology, Harvard Medical School; and a MacArthur Foundation Fellow. Her research on microglial cells — the immune cells of the central nervous system — has prompted a fundamental shift in thinking about neuron communication in the healthy brain and the origins of adult neurological diseases.
Until recently, it was believed that the primary function of microglia was immunological: they protect the brain by reducing inflammation and removing foreign bodies. Stevens and her colleagues have described a critical role of microglia in “pruning” or removal of extra synapses during normal brain development. This work is redefining our understanding of how the brain’s wiring forms and changes in early life, shedding new light on how the nervous and immune systems interact to determine adult neural circuitry. Stevens’s discoveries suggest that diseases caused by deficient neural architecture (such as autism and schizophrenia) or states of neurodegeneration (such as Alzheimer’s or Huntington’s disease) may be the result of impaired microglial function and abnormal activation of this pruning pathway.
Although synapse elimination is largely considered a developmental process, early synapse loss and dysfunction are increasingly recognized as a hallmark of many neurodegenerative diseases. However, the factors that trigger synapse loss in the aged and diseased brain remain elusive. In collaboration with investigators from the fields of human genetics and genomics, Stevens is pursuing the emerging hypothesis that synapse loss in neurodegenerative diseases is caused by a reactivation, in the mature brain, of developmental mechanisms of synapse elimination. Indeed, components of the complement cascade – molecules that signal to microglia and induce synaptic elimination – are profoundly upregulated in Alzheimer’s disease, glaucoma, and other brain diseases, and are localized to synapses prior to signs of neuronal loss in animal models.
Fengfeng Bei, Brigham and Women’s Hospital and Zhigang He, Boston Children’s Hospital
Zhigang He, PhD, BM, Bibliography
Featured Publications:
Nature (September 2018)
Touch and tactile neuropathic pain sensitivity are set by corticospinal projections.
Neuron (2017)
A Sensitized IGF1 Treatment Restores Corticospinal Axon-Dependent Functions
Neuron (May 2016)
Intrinsic Control of Axon Regeneration
Vector (January 2016)
Drug ‘cocktail’ could restore vision in optic nerve injury
Brain Regeneration
Thanks to work inspired by Zhigang He, PhD, a principal investigator at the Kirby Center, and Professor of Neurology and Ophthalmology at Harvard Medical School, the regrowth or repair of nerves in the central nervous system, once thought impossible, is within reach. Dr He’s work on axon regeneration has placed him among the most highly cited scientists in the world, according to Thomson Reuters.
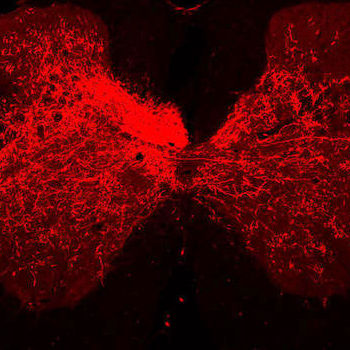
Functional deficits after spinal cord or other types of CNS injuries are primarily due to a disruption of axonal connections. Thus, to restore motor function after injury, what is needed is regeneration of the severed axons of long fiber tracts in order to re-establish the disrupted connections. The He Lab collaborates with the labs of Clifford Woolf and Larry Benowitz, together working to advance our fundamental understanding of the molecular processes underlying normal neuronal development. They apply this knowledge to incite injured nerves to recall their previous capabilities and restore themselves. In a 2017 paper, Dr. He and colleagues describe their success at promoting axon regrowth with functional recovery in mouse models after spinal cord injury or stroke.
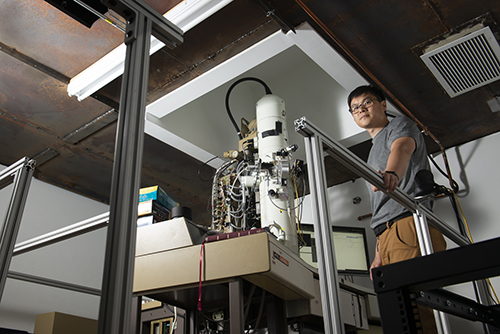
Photo by Anna Olivella, courtesy of the Harvard Brain Science Initiative.
Wei-Chung Allen Lee, PhD, Bibliography
Featured Publications:
Nature (April 2016)
Anatomy and function of an excitatory network in the visual cortex.
eLife (May 2017)
Wiring variations that enable and constrain neural computation in a sensory microcircuit.
Anatomy of Action
How do neural and network computations arise from neuronal circuits?
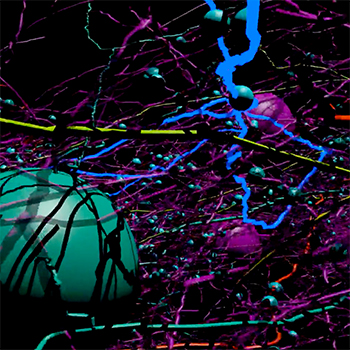
The long-term goal of the Lee Lab is to understand the organizational principles that underlie information processing in the circuits of the brain. The lab develops and deploys “functional connectomics” to discover the relationship between circuit structure and function in the Drosophila and rodent brain.
Using large-scale electron microscopy (EM) and in vivo multi-photon calcium imaging to examine the structure and function of neurons and networks, they unravel synaptic connectivity to uncover network motifs and understand the logic of circuit connectivity. In this way they can make inferences about how patterns of connectivity shape neuronal computations — reverse-engineering circuit mechanisms underlying thought and behavior.